Long-Term Disability Requirements Explained

Becoming disabled is understandably a stressful time for you and your family. Fortunately, if you have long-term disability (LTD) insurance through your employer, or even a policy that you purchased yourself, you have access to a percentage of your monthly earnings in the event that you cannot return to work. Your policy will outline the requirements that you will need to meet in order to qualify for long-term disability benefits. Policy language can vary, so it is important that you read your policy documents carefully when you are considering filing a long-term disability claim. We have highlighted some of the most common requirements for long-term disability benefits below.
Definition of Disability Requirements
In every long-term disability policy, there will be a definition of disability that you will need to meet in order to receive long-term disability benefits. Unfortunately, this is usually the requirement that insurance companies argue claimants do not meet and use as a basis to deny or terminate benefits. The definition of disability can vary from policy to policy and usually changes after a certain period of time, like 24 or 36 months. Typically, when you first become disabled, you will likely have to meet an “own occupation” definition of disability through the Elimination Period and, most commonly, the first 24 months of benefits. This definition usually requires you to prove that you are unable to perform the main duties of the job you were doing at the time you became disabled, as it is performed in the national economy.
Following the “own occupation” period, the definition of disability will likely change to “any occupation.” This means that in order to meet the definition of disability, you need to prove that you are unable to perform the main duties of any occupation. Depending on the policy language, this definition may take into consideration your prior work earnings and/or your training, education, and experience. This means that you may still meet the “any occupation” definition if you are unable to earn a certain percentage of your previous income or the insurer finds that you lack any skills that would transfer to an occupation you are able to perform with your restrictions and limitations. It is important to read the policy carefully and be mindful of when the definition of disability changes (if it does), so that you can provide the appropriate evidence to show you meet the correct definition.
https://cck-law.wistia.com/medias/1fvv2kr5p1?embedType=async&videoFoam=true&videoWidth=640
Appropriate Care and Treatment Requirements
Other common requirements when seeking long-term disability benefits include that you are receiving appropriate care and treatment from a physician. This means that you must be actively consulting and treating with a physician regarding your condition, undergoing testing when required, and taking any prescribed medications. In some instances, your doctor may have told you that there is nothing further they can do in order to improve your condition and discharge you from care. In this case, it is important to get a report from your doctor stating this opinion and continue to take your medications, perform home exercises, use heat and ice as needed, or anything else that your doctor has suggested in order to manage your condition.
Additionally, even if your doctor has discharged you, it may still be beneficial for your health and your claims to continue to check in with them, even on an annual basis, in case there are any changes in your condition or symptoms. Ultimately, it is important to have a good treating physician who is willing to support your long-term disability claim and maintain open communication with you about your health.
Comply with Insurer Requests
Lastly, the insurance company will routinely request claim forms, physician statements, or updated medical records in order to evaluate your claim and determine if you continue to meet the applicable definition of disability. A requirement of receiving long-term disability benefits is that you comply with these requests and provide the insurance company with the information it needs so that it can properly review your claim. If you do not provide this information, your claim will likely be denied or terminated since you have not provided continued proof of your disability. Additionally, these requests often have deadlines by which the insurance company needs this information. It is important that you meet the insurer deadlines or, if necessary, request an extension to submit this information. If you fail to provide the requested information in a timely manner, you may be at risk for your claim to be denied or terminated.
Further, the insurance company may at some point require you to undergo testing, such as an evaluation or an independent medical exam, in order to determine if you continue to meet the definition of disability. Though there are some circumstances where you may be able to object to this request, you are likely required to attend the appointment under the policy or potentially risk your claim being denied or terminated. Although these routine requests can be frustrating, it is important to work with the insurance company to provide detailed evidence in support of your disability, and hopefully make it easier for your claim to be continued.
Contact Chisholm Chisholm & Kilpatrick LTD
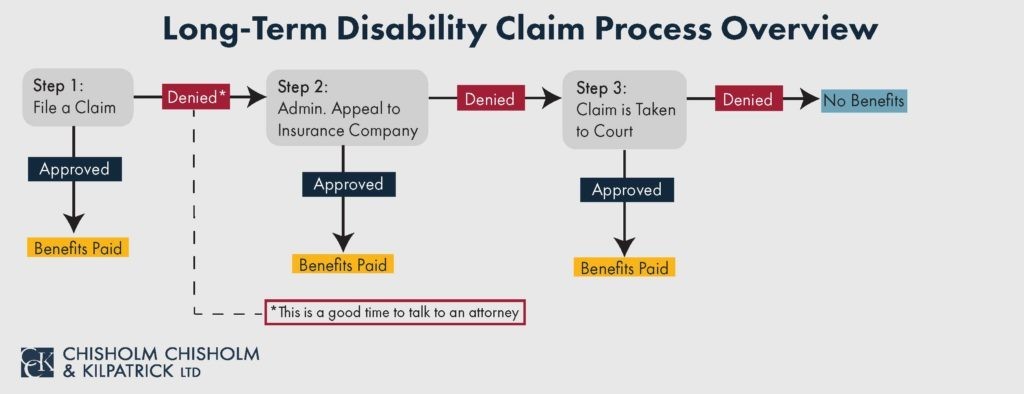
The attorneys and professionals at Chisholm Chisholm & Kilpatrick have extensive experience with and knowledge of the requirements commonly found in long-term disability policies. We can help you navigate the claims process and ensure that you are providing information that demonstrates you meet the definition of disability, are in appropriate care and treatment, complying with all requests from the insurance company, and meeting any other requirements found in your policy. Contact us today for a FREE consultation to see if we are able to assist you.
Share this Post